llustration: The human powered hospital. By Golnar Abbasi & Arvand Pourabbasi. Taken from Human Power Plant: Human Powered Neighbourhood, Melle Smets & Kris De Decker.
The environmental footprint of the health care sector
Health care is one of the most important economic sectors in high income countries, but its environmental footprint is underreported and not often considered. Most research into sustainable health care is less than five years old. A 2019 research paper calculated that the sector accounts for 2-10% of national carbon footprints across all OECD countries, China, and India, with an average share of 5.5% overall. [1-2]
The data refer to the year 2014, when the health care sectors of all these 36 countries combined were responsible for 1.6 Gt of greenhouse gas emissions. This corresponds to 4.4% of the global total emissions that year (35.7 Gt) – almost double the share of aviation. The US has the most carbon-intensive health care system, accounting for up to 10% of national carbon emissions. [3] It also produces 9% of national air pollution, 12% of acid rain, and 10% of smog formation nationally.
The environmental footprint of health care keeps increasing. For example, in the US, the health care sector’s greenhouse gas emissions grew by 30% between 2003 and 2013. [3] The rise in emissions couples an increase in spending – in fact, the emissions are often calculated based on spending. US national health expenditures as a percentage of Gross Domestic Product (GDP) increased from 3% in 1930, to 5% in 1960, to 10% in 1983, to 15% in 2002, and to 17.7% in 2019. [4-5] In the EU, health care spending per capita more than doubled between 2000 and 2018, and total spending is now at 9.9% of GDP. [6]
The 36 countries whose health care systems together cause 4.4% of global emissions only have 54% of the worldwide population. The remaining 46% of the population produces little or no health care related emissions because they don’t have access to health care. If we were to extend the OECD-China-India health care system globally, emissions would double to about 8% of the worldwide total. Furthermore, there are very large differences between these 36 countries. If the whole world were to copy the US health care system, the global carbon footprint of the health care sector would amount to around 16 Gt – almost half of total emissions worldwide in 2014.
Intense spotlights, high power medical equipment
What makes modern health care so resource-intensive? [7] To start with, modern hospitals are high energy users, primarily because of large plug loads from medical devices, lighting, ventilation and air-conditioning. [3, 8-12] In operating rooms, the high power use is mainly due to the use of intense spotlights and ultra clean ventilation canopies. In intensive care units and diagnostic imaging departments, medical equipment dominates the power load. [9]
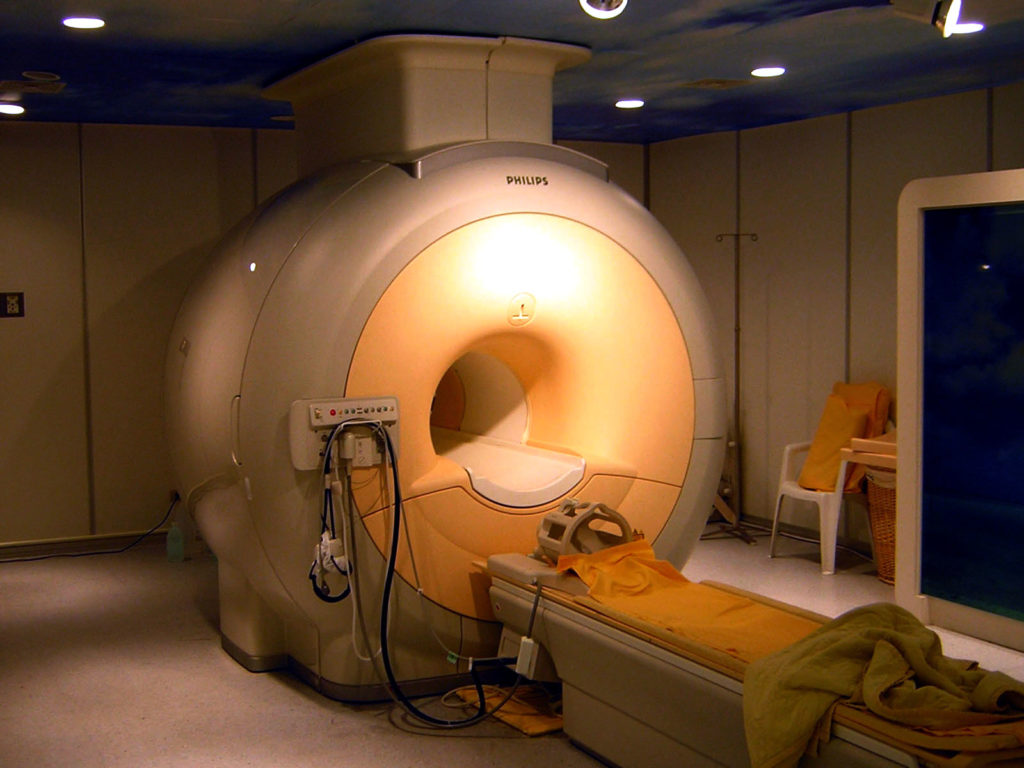
An MRI-scanner in Taipei, Taiwan (2006). Image: Kasuga Huang (CC BY-SA 3.0).
Like so many other sectors in modern society, health care has come to rely on all types of machines and devices. [13] Some of this medical equipment has very high power use. For example, an MRI-scanner, one of the most powerful diagnostic imaging technologies, can use as much electricity as more than 70 average European households. A 2020 study calculated that high-tech medical diagnostic technology (both MRI- and CT-scanners) was responsible for a whopping 0.77% of global carbon emissions in 2016. [14]
The power use of smaller medical equipment is poorly researched, but an inventory of two US hospitals showed that they had 14,648 and 7,372 energy using devices, of which the infusion pumps alone consumed more electricity on aggregate than an MRI-scanner. [13] The high density of medical equipment also increases the electricity use of air-conditioning in hospitals. [9]
Resource use along the supply chain
Even more energy – around 60% of the total – is used indirectly along the supply chain. [1,3,10,15]. This concerns the procurement of medical equipment, pharmaceuticals, and other medical products.
To start with, the growing number of medical devices used in hospitals also needs to be manufactured and brought to market. This requires activities such as the mining of resources and the construction and operation of research laboratories, factories and transport vehicles. This “embodied energy” of the medical equipment supply chain is very poorly researched. A study calculated that the production of an MRI-scanner requires more than half the fossil fuels used in the production of a passenger jet, and that the embodied energy is one third of the total energy use of the machine. [16]
Modern health care is also highly dependent on pharmaceuticals, which account for between 10 and 25% of total health care emissions, depending on the country. [15,17] A 2019 study revealed that the global pharmaceutical industry produces more greenhouse gases than the global automotive industry: 52 MtCO2 versus 46 MtCO2. [18] However, there is almost no data about the environmental footprint of specific pharmaceuticals, because corporate secrecy prevents scientists from making life cycle analyses.
Single-use disposable products are another source of health care energy use and pollution. [19-24] These products are worn by medical personnel and patients (face masks, gloves, overshoes, hats, drapes, gowns). Towels, basins, sterile plastic packaging, and utensils such as syringes, laryngoscopic handles and blades, anaesthetic breathing circuits, and even surgical instruments are also provided for single use. These disposable products are supplied to hospitals in so-called custom packs, which are sets of prepackaged sterile products for any specific medical procedure you can imagine. In principle, once a pack is opened, all items are discarded, even if they were not used.
When these practices are questioned, it is often for the hospital waste they create — the average patient in a hospital produces at least 10 kg of waste per day. [25] However, the environmental footprint increases significantly if the embodied energy and waste in the supply chain for making these disposable products is considered too. A study of cataract surgery in the UK – cataracts are the main cause of blindness worldwide – shows that the manufacturing of disposable materials accounts for more than half of the total carbon footprint of the procedure. [26]
Anesthetics & Vaccines
Finally, some specialist medical drugs produce emissions too. Inhalation anesthetics, which suppress the central nervous system and are a cornerstone of surgery, are potent greenhouse gases, which evaporate into the atmosphere after they have been inhaled by the patient (vented to the outside through the high energy ventilation systems of modern operating rooms). [27] Maintaining a 70 kg adult anesthetized for an hour produces from 25 kg (using isoflurane) to 60 kg (desflurane) CO2-equivalents, which corresponds to the emissions of driving an average European car (121gCO2/km) for 200-500 km (or driving it for around 4 hours). [15]
Pressurized dose inhalers, which are used to treat asthma and chronic obstructive pulmonary disease, also release potent greenhouse gases. Globally, around 800 million pressurized dose inhalers are manufactured annually, with a total carbon footprint that corresponds to the yearly emissions of more than 12 million passenger cars. [17,27] Vaccines are another key element of modern health care. They release carbon emissions not only through their development and production, but also by their resource-intensive distribution, which involves a dedicated cold chain. I could not find any reference to its environmental footprint.
Carbon footprint of medical procedures
Health care services often involve all of the above mentioned sources of emissions: medical devices, pharmaceuticals, and disposable materials. When the emissions in hospitals and along the supply chain are combined, it becomes possible to calculate the environmental footprint of medical procedures.
For example, studies of cataract surgery and reflux control surgery in the UK estimated the carbon footprint to be 182 kg and 1 ton of emissions, respectively, which corresponds to between 1,517 km and 8,333 km of driving. [28,29] Renal dialysis, a treatment to replace kidney function, produces 1.8 to 7.2 tonnes of emissions per patient per year, equal to the emissions of 15,000 to 60,000 km of driving. [28,30]
The limitations of carbon and energy efficiency
Although data on its environmental footprint is still incomplete, it seems quite clear that modern health care is not compatible with a transition to a low carbon society. The big question is whether or not this can be fixed without lowering the levels of care, pain relief, and longevity that people in high income societies have grown accustomed to.
Many efforts and studies into health care sustainability aim to reduce energy use and emissions without affecting the quality of medical treatments, often explicitly so. For example, the authors of a 2020 study into the Austrian health care system write that it’s “crucial to understand how the health care sector can reduce its emissions without undermining its service quality”. [17] Elsewhere, researchers write that “any solution that would reduce environmental impacts while reducing performance at the same time cannot be deployed”. [31]
As a consequence, many researchers tend to focus on improving carbon and energy efficiency. These strategies aim to deliver the same “performance” or “service quality” but with less energy (thanks to more energy efficient equipment), or with less emissions (owing to more renewable energy sources). [32]
The problem is that the quality of medical treatments continues to improve, resulting in extra energy use that erases the savings that result from carbon and energy efficiency. For example, in 2012 researchers calculated that MRI-scanners could be made 10-20% more energy efficient with relatively simple changes in design and operation. [31] Some of their proposed changes are now in use, but the energy use of MRI-scanners has not decreased, on the contrary.
A first reason is that MRI-scanners now come with higher field strengths (which offer diagnostic images of higher accuracy) and with larger boreholes (which improve patient comfort and allow obese or very muscular patients to be scanned). These innovations have improved the quality of care, but they have done so at the expense of extra energy use. In the 2012 study, the average power consumption per scan before the energy efficiency improvements was 15 kWh. A 2020 study measured an energy use of 17 kWh and 23.6 kWh per scan for an MRI-scanner with a field strength of 1.5 and 3 Tesla, respectively. [33]
Second, MRI-scanners with better diagnostic capabilities also increase energy use in unexpected ways, because medical equipment, pharmaceuticals, and treatments shape and change each other. [34] For example, doctors used to diagnose a patient through physical examination and communication, and only used diagnostic services to confirm the diagnosis, if necessary. Now, diagnostic tests happen upfront and drive the decision process, resulting in more tests and higher energy use. The introduction of new pharmaceuticals can foster increasingly energy-intensive diagnostic practices, too. For example, certain cancer treatment drugs are now being designed to treat a very specific tumor subtype, which requires more and more accurate medical imaging to identify the tumor subtype. [34]
Adding more renewable energy sources could potentially lower the emissions of health care both on-site and throughout the supply chain, but as the energy use of medical treatments continues to increase, this outcome is unlikely. Besides, a quick calculation shows that, even without further growth in energy use, a carbon neutral US health care system would gobble up the entire US renewable energy production – sun, wind, hydroelectric, wood, geothermal, biofuels, and waste. [35] The challenge is only slightly smaller in other high-income countries. Finally, renewable energy would not solve all of the health care sector’s environmental damage, and would not even eliminate all of its carbon emissions.
Sufficient health care?
To reduce the environmental footprint of modern health care, we need to question the trend towards ever greater reliance on energy-intensive technologies and services. The same holds true in other domains of life. [32]
However, while some people see the charm and real advantages of frugal and past ways of living when it comes to comfort or convenience, few would be tempted to apply the same principles to health and longevity. After all, the health care equivalent of travelling more slowly or wearing an extra sweater at home may be living a shorter life, suffering more pain, or being less mobile in old age. For example, if we would stop using MRI-scanners, or only use those with a field strength up to 1.5 Tesla, the lower diagnostic accuracy will lead to some cancers not being detected, resulting in lower cancer survival rates, and a lower average life expectancy. Or at least, so it seems.
The surgeon, a painting by David Teniers, 1670s.
Barber-surgeon extracting a tooth, a painting by Adriaen van Ostade, 1630.
If health care is viewed in a historical context, it seems clear that there is a powerful connection between the use of energy-intensive medical technologies on the one hand, and the health and longevity of a population on the other hand. Even looking back less than a century shows much lower health outcomes and survival rates for all kinds of diseases, and today’s global average life expectancy (72.6 years) is higher than in any high-income country back in 1950.
Hospitals date back to antiquity, but they merely welcomed those gone mad or awaiting death. In the middle ages, surgery happened at the barbershop, where “barber-surgeons” offered blood-letting, tooth extractions, and amputations alongside the more usual haircuts and shaves. They brew their own anesthetics based on herbs and alcohol, which could be just as deadly as the treatment itself. [36] A look at the “developing” world today also seems to suggest a clear connection between health care emissions, which are very modest, and life expectancy, which can be 20 to 30 years below that in high income countries. [37-41]
However, if one digs deeper, the connection between energy use and longevity is not as strong as it seems. This is proven by the USA, which has the most expensive and unsustainable health care system in the world, but ranks behind most European countries on the Health Care Access and Quality Index (which measures death rates from 32 causes of death that could be avoided by effective medical care). US citizens also have a lower life expectancy than European citizens. Clearly, there are other factors at play, too.
Resistance to disease
To start with, the quality of a health care system is not the only determinant of health and longevity. Here’s where history does have an important lesson to teach us. Medical knowledge dating back to antiquity viewed health in a more holistic way and placed great emphasis on building up the body’s inherent resistance to disease. For example, Hippocrates, often referred to as the father of Western medicine, prescribed diet, gymnastics, exercise, massage, hydrotherapy, and swimming in the sea. [42]
One could argue that our forebears had no other choice than to focus on preventing disease, because they had few treatments available. However, the wisdom of their approach is more obvious than ever. Nowadays in high income societies, many patients need medical treatment because of so-called lifestyle diseases – those caused by poor or excessive nutrition, lack of physical activity, stress, or substance abuse. Typical health risks are cardiovascular disease, diabetes type 2, depression, obesity, some types of cancers, and higher susceptibility to infectious diseases. Industrial society has given us effective medical treatments, but it’s also making us sick.
This means that health and longevity can be promoted in other ways than through an increasingly resource-intensive health care system. By addressing the broader determinants of health and longevity, we could make a switch from curative to preventive medicine. [15,43] Preventive medicine is not about the government telling us not to smoke (and then cashing in tax money on the sales of cigarettes). Rather, it concerns systemic changes that go beyond behavioural change.
Rush hour in São Paulo, Brazil, 2005. Public domain.
For example, significantly reducing the use of cars in our societies would bring a surprisingly large number of health benefits that would lower the need for energy-intensive medical treatments. It would decrease the health damage done through traffic accidents and through air and noise pollution. It would make people more physically active (preventing many lifestyle diseases), and it would free a lot of public space for people to come together, for kids to play, and for trees to grow (all important factors for the mental health of a population). Finally, reducing the use of cars may easily save more greenhouse gas emissions than the health care system produces.
Switching to a healthier food production system, addressing the environmental damage done by the plastic industry, reducing poverty and social inequality, introducing shorter work hours, and more meaningful jobs are other examples of preventive medicine. We have not achieved the higher life expectancy of today only because of better health care systems. We also got it because of better education, sanitation, safety and traffic regulations, welfare systems, crime control, and a more reliable food supply. The low average life expectancy in poor countries is also partly due to these factors.
Preventive medicine would also reduce the health damage done by the medical treatments themselves. This concerns health damage resulting from medical errors or side effects of pharmaceuticals and more indirectly from the pollution that the health care sector generates. For example, air pollution from health care services contributes to the prevalence of asthma, which in turn increases the demand for health care. Climate change and other environmental damage threaten younger and future generations with even larger health impacts, for example through crop failures, spread of diseases, extreme weather events, and natural disasters. [44]
The law of diminishing returns
Second, within a health care system, medical practices with higher energy use do not necessarily lead to increased health outcomes in a proportional way. Like so many other sectors in industrial society, curative health care is vulnerable to the law of diminishing returns: it takes ever more energy to gain ever smaller increases in health outcomes. [5] Conversely, this means that a relatively small decline in the quality or specifications of medical treatments could yield comparably large reductions in resource use and emissions.
Infection control is a good example. The development of general anesthesia in the 1840s made surgery possible, but at the time over 90% of surgical wounds became infected, often leading to death. [45] The first major decrease in infection rates followed antiseptic practices (1880-1900), and the second followed the introduction of antibiotics (1945-1970). By 1985, the overall infection rate had decreased to about 5%. Since then, a lot of resources have been invested to achieve incremental gains towards 100% sterility, mainly by replacing reusable supplies by single-use, disposable products. [26]
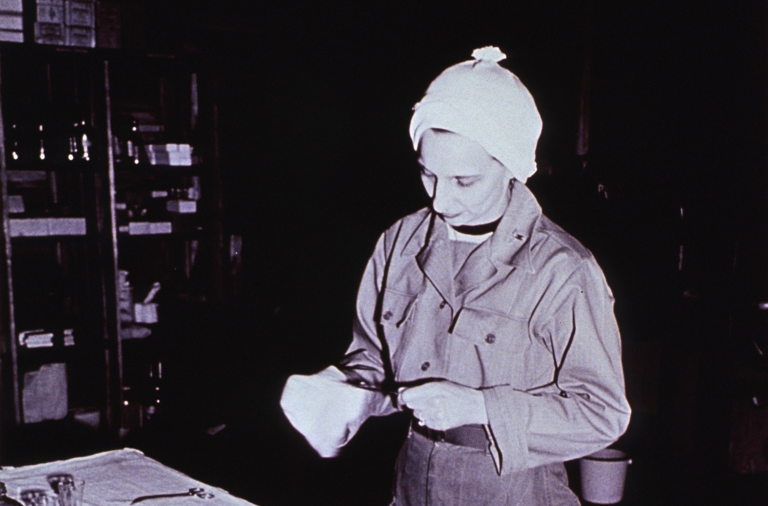
Operating room nurse preparing instruments for surgery at the 3rd Station Hospital, Korea. 1951. Source: US National Library of Medicine.
If properly decontaminated, reusable supplies carry no increased infection risks, but cross-contamination between patients sometimes happens by mistake. Nevertheless, some scientists have advocated for a return to reusable products, which have a much lower environmental footprint in most cases. For example, the use of reusable laryngoscope handles produces 16-25 times less greenhouse gases than single-use, disposable ones. [45]. The researchers admit that their approach may increase deaths from surgical infections. Still, they argue that the health damage caused by the production of single-use disposable supplies is even more considerable.
When it comes to maximizing returns, less affluent societies can teach us some lessons. Comparisons of cataract surgery in the UK and in India have shown that the same treatment (phacoemulsification) in India’s Aravind Eye Clinics is much cheaper and produces only 5% of the emissions and 6% of the solid waste in the UK. This is mainly because the Indian surgeons reuse as many supplies, devices, and drugs on as many patients as possible. [26,46-49] In addition, they use locally manufactured supplies, implants, and drugs, and they apply a dual-bed system in which one patient is operated while another one is being positioned and prepared in the bed next to it.
Although these practices flout regulations for infection control in high income countries, cataract surgery in India achieves similar or better outcomes and does not cause any more infections than it does in the UK or the US. [26,46-49] Consequently, it may well be that the law of diminishing returns has reached its ultimate limit, in the sense that an expensive and unsustainable medical practice does not seem to bring any health benefits at all. The Indian eye clinics demonstrate that an effective model of care is possible without expensive and unsustainable supplies and resources. Medical innovation can happen without new technology.
Driven by profit
The law of diminishing returns and the focus on curative medicine are both rooted in the fact that medical innovation is primarily driven by profit. [50,51] Private companies who develop and sell medical equipment, pharmaceuticals, and other health care products have nothing to win or earn if the demand for new curative health care technologies and products declines, or if medical technologies were to be judged in relation to their resource use. The medical industry — logically — wants to increase the sales of its products, and has enormous marketing budgets and lobbying power at its disposal to achieve that goal. [52]
King George Military Hospital, electrical treatment and x-ray room. 1915. Source: US National Library of Medicine.
The WHO estimates that 20-40% of health care spending is wasted, and argues that “the cost-effectiveness, real need, and likely usefulness of many innovative technologies are questionable”. [44, 37] An increasing body of academic literature shows the extent to which patients in high income countries are “overdosed, overtreated, and overdiagnosed”. [44, 14]
None of this is inevitable. A modern health care system could also work in another economic context. For example, some have suggested the open source development of medical equipment and pharmaceuticals, in which health care technology would become a commons. Shifting the tax burden from labour to resources could be another part of the solution. In high income countries, medical equipment, pharmaceuticals, and disposable products partly serve to reduce the expensive human labour force in health care.
Age and Sustainability
Based on the fragmented data available, it seems likely that the resource use of modern health care systems could be reduced significantly, without bringing us back to the barber-surgeons of the middle ages. A health care system that is more focused on preventive medicine, and which operates outside the logic of the market, could reduce emissions without negatively impacting health, maybe even improving it.
Otherwise, the law of diminishing returns highlights opportunities to lower the environmental footprint of health care services. For example, if the environmental footprint of health care was halved, it’s very unlikely that life expectancy would decrease proportionally. Nearly half of lifetime health care expenditures – and thus energy use and emissions – is incurred during the senior years (+65 years old). For those up to age 85, more than one-third of their lifetime expenditures will accrue in the remaining years. [53]
Advocating for a shorter average life expectancy, even if it may concern a very modest decrease, sounds problematic. However, avoiding the topic is just as problematic. Because of modern health care’s enormous (and still growing) environmental footprint, today’s health and longevity comes at least partly at the expense of the health and longevity of younger and future generations, who have no voice in this debate. [44]
If we cure one person today, at the expense of making other people sick tomorrow, health care becomes counter-productive. Health is not only a private good but also a public one, and as medical treatments become increasingly resource-intensive, the chances grow that the public health damage of a treatment outweighs the individual gain of a patient, especially at old age.
Kris De Decker
Thanks to Elizabeth Shove
Proofread by Alice Essam & Eric Wagner
References
[1] Pichler, Peter-Paul, et al. “International comparison of health care carbon footprints.” Environmental Research Letters 14.6 (2019): 064004. https://iopscience.iop.org/article/10.1088/1748-9326/ab19e1/pdf
[2] National estimates of health care sector greenhouse gas emissions have been performed for the UK (2009), the USA (2009 & 2016), Sweden (2017), Australia (2018), Canada (2018), China (2019), Japan (2020) and Austria (2020). For an overview, see [15]. However, because each study has its own methodology, the results are not perfectly comparable. That’s why I quote this source, as it gives comparable estimates.
[3] Eckelman, Matthew J., and Jodi Sherman. “Environmental impacts of the US health care system and effects on public health.” PloS one 11.6 (2016): e0157014. https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0157014
[4] US National Health Expenditure Data. Centers for Medicare & Medicaid Services. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/NationalHealthAccountsHistorical
[5] Tainter, Joseph. The collapse of complex societies. Cambridge university press, 1988. Page 102 & 103.
[6] Current healthcare expenditure, 2012-2017, Eurostat. Current health expenditure per capita (current US$) – European Union, World Bank. Current health expenditure per capita, PPP (current international $) – European Union, World Bank. Health spending, OECD.
[7] In what follows, I ignore the resource use and emissions caused by transportation to and from health care facilities, as well as the resource use and emissions caused by the building of the health care facilities themselves.
[8] Research in different countries has shown an electricity use of 130 to 280 kilowatt-hour per square metre per year, representing around 50% of total on-site building energy consumption. [11-12] For comparison, residential electricity use in European households is on average 70 kWh/m2/year, and total energy demand is dominated by heating, not electricity. According to a 2016 study, for which scientists collected power data over a period of 18 months in a German hospital, operating rooms have the highest electricity use (438 kWh/m2/year), followed by intensive care units (135 kWh/m2/yr). [9]
[9] Christiansen, Nils, Martin Kaltschmitt, and Frank Dzukowski. “Electrical energy consumption and utilization time analysis of hospital departments and large scale medical equipment.” Energy and Buildings 131 (2016): 172-183.
[10] Wu, Rui. “The carbon footprint of the Chinese health-care system: an environmentally extended input–output and structural path analysis study.” The Lancet Planetary Health 3.10 (2019): e413-e419. https://www.sciencedirect.com/science/article/pii/S2542519619301925
[11] Bawaneh, Khaled, et al. “Energy consumption analysis and characterization of healthcare facilities in the United States.” Energies 12.19 (2019): 3775. https://www.mdpi.com/1996-1073/12/19/3775/pdf
[12] Rohde, Tarald, and Robert Martinez. “Equipment and energy usage in a large teaching hospital in Norway.” Journal of healthcare engineering 6 (2015). http://downloads.hindawi.com/journals/jhe/2015/231507.pdf
[13] Black, Douglas R., et al. “Evaluation of miscellaneous and electronic device energy use in hospitals.” World Review of Science, Technology and Sustainable Development 10.1-2-3 (2013): 113-128. https://www.osti.gov/servlets/purl/1172701
[14] Picano, Eugenio. “Environmental sustainability of medical imaging.” Acta Cardiologica (2020): 1-5. https://www.tandfonline.com/doi/abs/10.1080/00015385.2020.1815985
[15] Sherman, Jodi D., et al. “The Green Print: Advancement of Environmental Sustainability in Healthcare.” Resources, Conservation and Recycling 161 (2020): 104882. https://www.researchgate.net/profile/Brett_Duane/publication/343137350_The_Green_Print_Advancement_of_Environmental_Sustainability_in_Healthcare/links/5f216962299bf134048f8960/The-Green-Print-Advancement-of-Environmental-Sustainability-in-Healthcare.pdf
[16] Martin, Marisa, et al. “Environmental impacts of abdominal imaging: a pilot investigation.” Journal of the American College of Radiology 15.10 (2018): 1385-1393. https://www.sciencedirect.com/science/article/abs/pii/S1546144018308639. The researchers write that “when production and use phases are combined, the total energy consumption of MRI (>309 MJ/examination, abdominal scan, 1.5 Tesla) is comparable with cooling a three-bedroom house with central air-conditioning for a day”.
[17] Weisz, Ulli, et al. “Carbon emission trends and sustainability options in Austrian health care.” Resources, Conservation and Recycling 160 (2020): 104862.
[18] Belkhir, Lotfi, and Ahmed Elmeligi. “Carbon footprint of the global pharmaceutical industry and relative impact of its major players.” Journal of Cleaner Production 214 (2019): 185-194. https://www.sciencedirect.com/science/article/abs/pii/S0959652618336084
[19] Laufman, Harold, Luther Riley, and Barry Badner. “Use of disposable products in surgical practice.” Archives of Surgery 111.1 (1976): 20-26. https://jamanetwork.com/journals/jamasurgery/article-abstract/581229
[20] Gilden, Daniel J., K. N. Scissors, and J. B. Reuler. “Disposable products in the hospital waste stream.” Western journal of medicine 156.3 (1992): 269. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1003232/pdf/westjmed00091-0045.pdf
[21] Sherman, Jodi D., and Harriet W. Hopf. “Balancing infection control and environmental protection as a matter of patient safety: the case of laryngoscope handles.” Anesthesia & Analgesia 127.2 (2018): 576-579. https://www.researchgate.net/profile/Jodi_Sherman/publication/322407715_Balancing_Infection_Control_and_Environmental_Protection_as_a_Matter_of_Patient_Safety_The_Case_of_Laryngoscope_Handles/links/5a82ba12a6fdcc6f3eadcfab/Balancing-Infection-Control-and-Environmental-Protection-as-a-Matter-of-Patient-Safety-The-Case-of-Laryngoscope-Handles.pdf
[22] Thiel, Cassandra Lee, et al. “Life cycle assessment of medical procedures: Vaginal and cesarean section births.” 2012 IEEE International Symposium on Sustainable Systems and Technology (ISSST). IEEE, 2012.
[23] Campion, Nicole, et al. “Sustainable healthcare and environmental life-cycle impacts of disposable supplies: a focus on disposable custom packs.” Journal of Cleaner Production 94 (2015): 46-55.
[24] “Reusables, Disposables each play a role in preventing cross-contamination”, Elizabeth Srejic, Infection Control Today, April 2016
[25] Sustainability roadmap for hospitals, American Association of Hospitals. http://www.sustainabilityroadmap.org/topics/waste.shtml#.YCsEOXyYXWc.
[26] Thiel, Cassandra L., et al. “Cataract surgery and environmental sustainability: waste and lifecycle assessment of phacoemulsification at a private healthcare facility.” Journal of Cataract & Refractive Surgery 43.11 (2017): 1391-1398. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5728421/
[27] Vollmer, Martin K., et al. “Modern inhalation anesthetics: potent greenhouse gases in the global atmosphere.” Geophysical Research Letters 42.5 (2015): 1606-1611. https://agupubs.onlinelibrary.wiley.com/doi/full/10.1002/2014GL062785
[28] Salas, Renee N., et al. “A pathway to net zero emissions for healthcare.” bmj 371 (2020).
[29] Brown, Lawrence H., et al. “Estimating the life cycle greenhouse gas emissions of Australian ambulance services.” Journal of Cleaner Production 37 (2012): 135-141.
[30] Connor, A., R. Lillywhite, and M. W. Cooke. “The carbon footprint of a renal service in the United Kingdom.” QJM: An International Journal of Medicine 103.12 (2010): 965-975. https://academic.oup.com/qjmed/article/103/12/965/1584174
[31] Herrmann, C., and A. Rock. “Magnetic resonance equipment (MRI)–Study on the potential for environmental improvement by the aspect of energy efficiency.” PE INTERNATIONAL AG, Report (2012).
[32] Shove, Elizabeth. “What is wrong with energy efficiency?.” Building Research & Information 46.7 (2018): 779-789. https://www.tandfonline.com/doi/pdf/10.1080/09613218.2017.1361746
[33] Heye, Tobias, et al. “The energy consumption of radiology: energy-and cost-saving opportunities for CT and MRI operation.” Radiology 295.3 (2020): 593-605. https://pubmed.ncbi.nlm.nih.gov/32208096/
[34] Blue, Stanley. “Reducing demand for energy in hospitals: opportunities for and limits to temporal coordination.” Demanding Energy. Palgrave Macmillan, Cham, 2018. 313-337.
[35] https://www.eia.gov/tools/faqs/faq.php?id=92&t=4
[36] Duffin, Jacalyn. History of medicine: a scandalously short introduction. University of Toronto Press, 2010.
[37] WHO compendium of innovative health technologies for low-resource settings, WHO; 2016-17. WHO, 2018. https://www.who.int/medical_devices/publications/compendium_2016_2017/en/
[38] Medical devices: managing the mismatch: an outcome of the priority medical devices project: methodology briefing paper, WHO, 2010. https://apps.who.int/iris/handle/10665/70491
[39] Global Atlas of Medical Devices, WHO, 2017. https://www.who.int/medical_devices/publications/global_atlas_meddev2017/en/
[40] Page, Brandi R., et al. “Cobalt, linac, or other: what is the best solution for radiation therapy in developing countries?.” International Journal of Radiation Oncology* Biology* Physics89.3 (2014): 476-480.
[41] In a survey of surgeons across 30 African nations, 48% reported at least weekly power failures, 29% had operated using only mobile phone lights, and 19% had experienced poor surgical outcomes as a result of it. [28]
[42] Parker, Steve. Medicine: The Definitive Illustrated History. DK Publishing, 2016.
[43] Hall, Peter A., and Michèle Lamont, eds. Successful societies: How institutions and culture affect health. Cambridge University Press, 2009.
[44] Borowy, Iris, and Jean-Louis Aillon. “Sustainable health and degrowth: Health, health care and society beyond the growth paradigm.” Social Theory & Health 15.3 (2017): 346-368.
[45] Sherman, Jodi D., and Harriet W. Hopf. “Balancing infection control and environmental protection as a matter of patient safety: the case of laryngoscope handles.” Anesthesia & Analgesia 127.2 (2018): 576-579.
[46] Steyn, A., et al. “Frugal innovation for global surgery: leveraging lessons from low-and middle-income countries to optimise resource use and promote value-based care.” The Bulletin of the Royal College of Surgeons of England 102.5 (2020): 198-200. https://publishing.rcseng.ac.uk/doi/pdf/10.1308/rcsbull.2020.150
[47] Haripriya, Aravind, David F. Chang, and Ravilla D. Ravindran. “Endophthalmitis reduction with intracameral moxifloxacin in eyes with and without surgical complications: Results from 2 million consecutive cataract surgeries.” Journal of Cataract & Refractive Surgery 45.9 (2019): 1226-1233. https://www.aurolab.com/images/JCRS%202%20million.pdf
[48] Venkatesh, Rengaraj, et al. “Carbon footprint and cost–effectiveness of cataract surgery.” Current opinion in ophthalmology 27.1 (2016): 82-88.
[49] Thiel, Cassandra L., et al. “Utilizing off-the-shelf LCA methods to develop a ‘triple bottom line’auditing tool for global cataract surgical services.” Resources, Conservation and Recycling 158 (2020): 104805.
[50] Relman, Arnold S. “The new medical-industrial complex.” New England Journal of Medicine 303.17 (1980): 963-970. https://www.nejm.org/doi/full/10.1056/NEJM198010233031703
[51] Smith, Richard. “Limits to medicine. Medical nemesis: the expropriation of health.” Journal of Epidemiology & Community Health 57.12 (2003): 928-928. https://jech.bmj.com/content/57/12/928
[52] In health care, there is a thin line between marketing and corruption, especially when the target audience is medical personnel that may gain benefits from using or prescribing a medical device or drug, or when regulators are influenced to facilitate practices that increase profits. Transparancy International ranks the procurement of drugs and medical equipment fourth on a list of seven processes that carry high risk of corruption, and calls the problem “widespread in all countries”. [37]
[53] Alemayehu, Berhanu, and Kenneth E. Warner. “The lifetime distribution of health care costs.” Health services research 39.3 (2004): 627-642. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1361028/